Analytics For Employers: A Tutorial (Part 1)
DataHealthcare
It’s been almost 3 years since we started BetaXAnalytics with the goal of using data science to offer strategic guidance to employers and providers on healthcare spending and services. Since opening our doors, we’ve spent a lot of time talking with companies who pay for healthcare for their employees, as well as the brokers and consultants who help to guide these decisions. At the same time, we’ve spent time taking a look at many of the analytic tools that are on the market right now—these are the technology platforms that provide spending transparency to employers and their brokers.
From day 1 when we started these customer interviews, one resounding theme was apparent. The biggest question we heard from employers and their brokers is simply this: Having data is good…but what do you do with it?
3 years later, this is still the most common question we hear. We see this recurring question from employers and their brokers as a symptom of the early-stage maturity of the employer health analytics market. In short, over the past decade as more self-insured employers use health data to help to manage their spending, we haven’t moved too far from the starting line.
Anyone who is familiar with the general progression of analytics will recognize the analytic maturity model below.

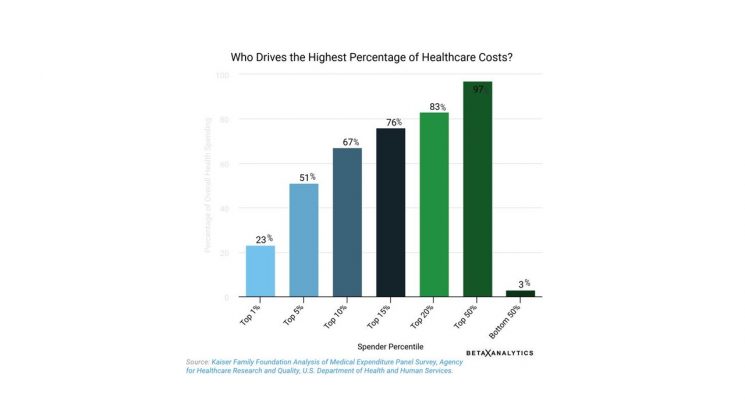
At its most basic level, health care analytics is often pigeonholed into “counting things.” Counting dollars, counting medications, counting members…and watching these numbers go up and down. So every time we get the question, “What do you do with the data?” this just reaffirms that most employers are still in the dark with respect to using data to drive their benefits strategy. This type of “analytics” examines only the past and gives very little insight into the 4 critical areas of focus as a healthcare purchaser (which we explain in Part 2 of this post).
After seeing many of the analytic tools on the market today, we can confidently assert that that the market for using health analytics to control employer healthcare spending is here:

Having data is good…but what do you do with it? This recurring question is a symptom of the low analytic maturity of the current state of employer health analytics—that is to say, we pay for access to data, but it’s rarely actionable. “Analytics” in this stage is synonymous with “counting” and data is hindsight-focused on reporting what has already happened.
The current state of employer analytics is a good start, but it barely scratches the surface of the strategic potential of analytics. Tracking spending is important, but true analytics go far beyond just spending to understand insights into your population health, designing and tracking programs to target conditions and support mental health, and even to provide insight into how well benefits are being communicated to employees. When we move past hindsight analytics to incorporate insight and foresight, we move past counting things, and to the realm of strategic benefit planning. This means developing a deeper understanding of who associates are, the benefits that will attract the best talent, and identifying the optimal strategy for funding these next-generation benefits packages. As with so many initiatives that fall under the Human Resources / Human Capital umbrella—including talent acquisition and retention, compensation, healthcare, engagement, benefits, wellbeing—the most strategic analytics should consider all of these areas. This is the future of analytics—and the future is here.
About BetaXAnalytics:
We combine data science with clinical, pharmacy and wellness expertise to guide employers and providers into a data deep-dive that is more comprehensive than any data platform on the market today. BetaXAnalytics uses the power of their health data “for good” to improve the cost and quality of health care. For more insights on using data to drive healthcare, pharmacy and wellbeing decisions, follow BetaXAnalytics on Twitter @betaxanalytics, Facebook @bxanalytics and LinkedIn at BetaXAnalytics.